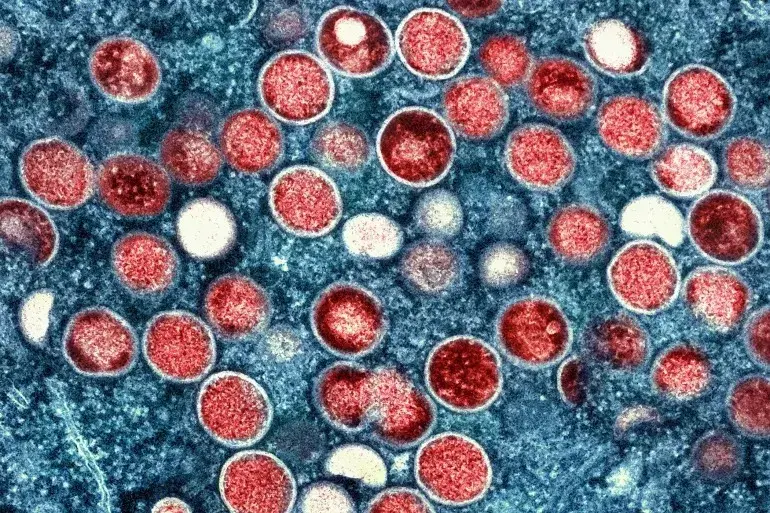
India Records First Suspected Mpox Case; Patient in Isolation After International Travel
India has recorded its first suspected case of mpox, a virus formerly known as monkeypox, in a young male patient who recently traveled from a country experiencing an outbreak. The health ministry announced that the patient is currently isolated in a hospital and is in stable condition, with ongoing measures to manage the case in …
India Records First Suspected Mpox Case; Patient in Isolation After International Travel Read More »